Kimberly G. Blumenthal MD, MSc, Tyler Harkness BS, Elizabeth J. Phillips MD, Allison Ramsey MD, Aleena Banerji MD, Upeka Samarakoon PhD, MPH, Cosby Stone MD, MPH, Xiaoqing Fu MS, David A. Khan MD, Iris Otani MD, Carlos A. Camargo Jr. MD, DrPH, Yuqing Zhang Dsc, Karen Donelan ScD, and the USDAR Study Team
Summary
Proper medical care for drug allergies relies on patients seeking out care at an allergy clinic, going to appointments with an allergist, and often undergoing testing for their allergies. However, very few people have access to care from an allergist, and those who do only rarely seek out proper allergy care. In order to improve care and spread allergy evaluations to all patients who need them, clinicians need to know more about the motivations and concerns of patients who choose to have an allergy evaluated.
Toward this goal, USDAR investigators analyzed all participants enrolled in the registry before January 2020. The data showed that the most common primary concern for drug allergy patients was the ability to use the best medication when they get sick. Additionally, many people reported their primary concern about having an allergic reaction again in the future. With this study serving as a foundation, USDAR and studies like it can keep building toward a full knowledge base on drug allergies and the people who have them, developing and enabling comprehensive, patient-focused care.
Abstract
Of 592 patients (mean age, 49 [standard deviation, 17] years, 74% female, 88% white), the most commonly reported drug allergies were penicillins (78%), cephalosporins (12%), and sulfonamides (12%) with common reactions of rash (62%), hives (54%), itching (48%), flushing or facial redness (28%), and swelling or angioedema (24%). Patient concerns, coded from freetext, were optimal medication use (41%), no concern (17%), allergic reaction(14%), diagnosis(12%), and severe allergic reaction(12%). Using multinomial regression, the presence of drug allergy concerns increased with greater age, higher number of reported drug reactions, more antibiotic use, and certain reaction symptoms, most notably mouth or palate itching. Female sex was associated with increased severe allergic reaction concern. Poorer general and mental health was associated with increased allergic reaction concern.
Patients with drug allergy were concerned about their options for medical treatment, having an allergic reaction, and receiving clarity about their diagnosis. Capturing and addressing patient concerns may improve the approach to patients with drug allergy and/or the effectiveness of drug allergy testing.
Figure – Associations between Primary Concerns about Drug Allergy and Patient Characteristics
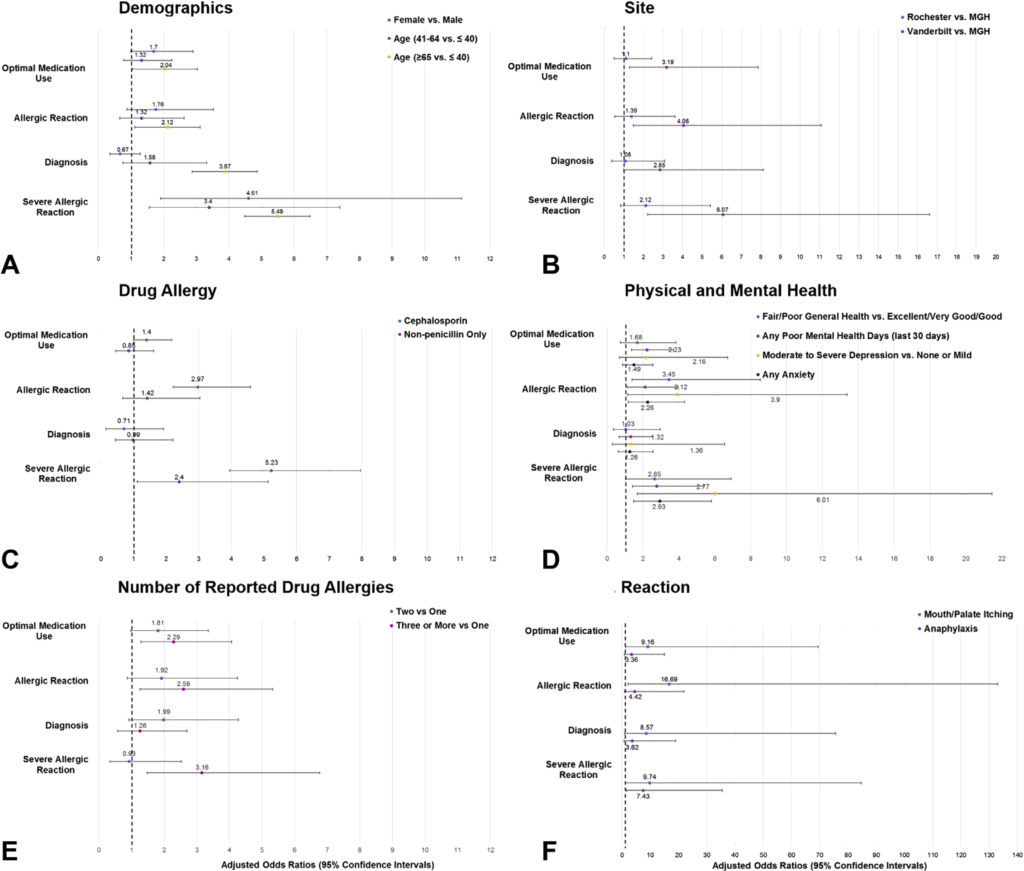
Select characteristics associated with patient concerns from multinomial regression models considering patient-reported primary drug allergy concerns, compared with no concern, which was the reference category. A, Demographics; B, Site; C, Drug Allergy; D, Physical and Mental Health; E, Number of Reported Drug Allergies; F, Reaction. MGH, Massachusetts General Hospital; RRH, Rochester Regional Health; USDAR, United States Drug Allergy Registry; VUMC, Vanderbilt University Medical Center.
Figure – Selection of Primary Concerns
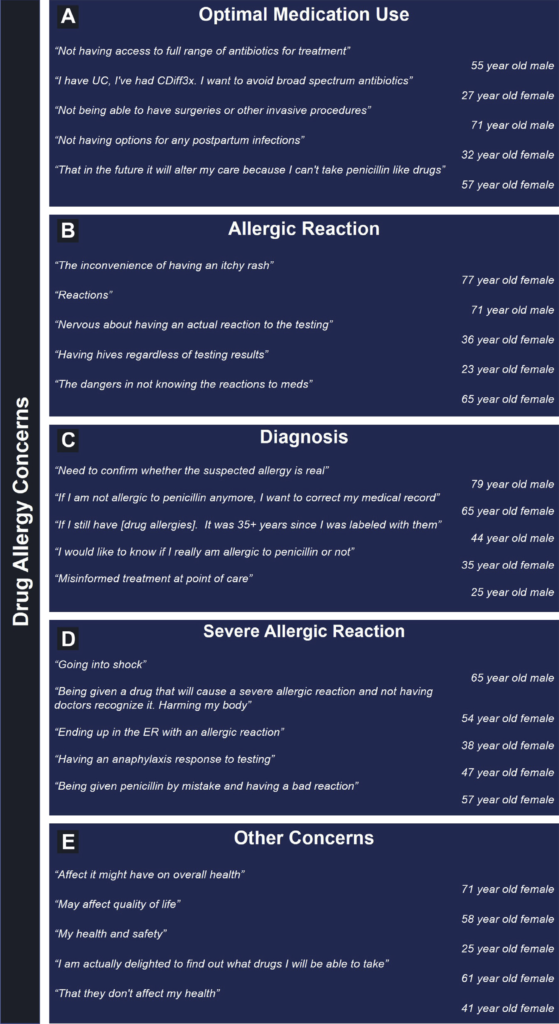
Free-text examples of patient-reported concerns by code: (A) Optimal Medication Use, (B) Allergic Reaction, (C) Diagnosis, (D) Severe Allergic Reaction, and (E) Other.